Eager to know pregnancy related frequently asked questions? Well, that’s so natural. Finding out you’re pregnant is an incredible moment—exciting, emotional, and maybe even a little overwhelming. Whether this is your first pregnancy or not, the first trimester comes with so many changes and, naturally, a lot of questions.
What should I eat? Is this symptom normal? When will I hear my baby’s heartbeat? It’s completely okay to feel unsure—that’s why your doctor is there! Asking the right questions early on can give you peace of mind and help you make informed decisions for a healthy pregnancy.
To make things easier, we’ve put together a comprehensive list of 20+ pregnancy related frequently asked questions you must ask your doctor. From prenatal care to lifestyle changes, this guide will help you navigate this beautiful journey with confidence. Let’s dive in!
Pregnancy Questions to Ask During the First Trimester
The first trimester is a time of rapid change—both for your baby and your body. From the moment you find out you’re pregnant, you may experience excitement, uncertainty, and a flood of questions. This stage is crucial and toughest for early prenatal care, lifestyle adjustments, and understanding what’s normal versus what requires medical attention.
Here, we cover the most important pregnancy related frequently asked questions to ask your doctor to ensure a healthy start to your pregnancy/. This way you’ll also learn some things to do during the first trimester of your pregnancy.
1. What is My Due Date?
Your due date is an estimate of when you will give birth, typically calculated as 40 weeks from the first day of your last menstrual period (LMP). This method assumes a 28-day cycle, with ovulation occurring around day 14. If you know the exact date of conception, your due date would be 38 weeks from conception.
However, since not everyone has a textbook cycle, your healthcare provider may use an ultrasound (typically done between 8-12 weeks) to get a more accurate estimate based on the baby’s size and development.
2. How Often Should I Schedule Prenatal Appointments?
General Appointment Timeline
The frequency of prenatal checkups varies based on pregnancy progression and maternal and fetal health. Below is the standard schedule:
- Weeks 4–28: Visits occur once every four weeks (monthly).
- Weeks 28–36: Appointments increase to every two weeks (bi-monthly).
- Weeks 36–41: Weekly check-ins take place until delivery.
Factors That May Affect Appointment Frequency
Certain conditions may require more frequent monitoring:
- Medical Risk Factors: Advanced maternal age (35+), pre-existing health concerns, or carrying twins or more.
- Pregnancy Complications: A history of pregnancy-related issues or the development of conditions like gestational diabetes or preeclampsia.
- Extended Pregnancy: If the pregnancy continues beyond 40 weeks, additional monitoring may be necessary.
Additional Considerations
- The initial prenatal visit is typically the most in-depth.
- Attending all scheduled appointments is essential, even if you feel fine.
- Routine checkups include monitoring weight, blood pressure, urine, and the size of the uterus.
- These visits provide essential medical evaluations, guidance, and emotional support throughout pregnancy.
3. Should I Take Prenatal Vitamins?
Yes! Prenatal vitamins are essential for a healthy pregnancy because they provide key nutrients that support your baby’s growth. The most important nutrients include:
- Folic Acid (400-800 mcg daily): Helps prevent neural tube defects (serious brain and spine abnormalities).
- Iron (27 mg daily): Supports increased blood volume and prevents anemia.
- Calcium (1000 mg daily) & Vitamin D: Essential for baby’s developing bones and teeth.
- DHA & Omega-3s: Supports brain and eye development.
Even if you eat a balanced diet, prenatal vitamins help fill any nutritional gaps to ensure your baby gets the necessary nutrients.
4. Should I Take Any Supplements?
Beyond prenatal vitamins, some women may benefit from additional supplements:
- Omega-3 fatty acids (DHA & EPA): Helps with baby’s brain and eye development.
- Vitamin B6: This can help reduce nausea and morning sickness.
- Probiotics: They may support digestion and reduce constipation.
Always check with your doctor before adding any supplements, as some may not be safe during pregnancy.
5. What Medications are Safe During Pregnancy?
Many over-the-counter and prescription medications should be avoided during pregnancy. However, some are considered safe when taken as directed:
- For pain/fever: Acetaminophen (Tylenol) is generally safe.
- For heartburn: Tums, Rolaids, and Pepcid AC.
- For nausea: Vitamin B6 and Unisom (Doxylamine) may help.
- For allergies: Benadryl, Claritin, and Zyrtec.
- For constipation: Fiber supplements, Colace (stool softener).
Medications to avoid: Ibuprofen (Advil, Motrin), aspirin, decongestants (like Sudafed), and certain antibiotics. Always consult your doctor before taking any medication during pregnancy.
6. How Can I Treat Morning Sickness?
Morning sickness (nausea and vomiting) is common in the first trimester due to hormonal changes. Some ways to relieve it include:
- Eating small, frequent meals instead of three large meals.
- Avoiding greasy, spicy, and strong-smelling foods.
- Keeping crackers, toast, or dry cereal on hand.
- Drinking ginger tea or sucking on ginger candies.
- Staying hydrated by sipping water, clear broth, or electrolyte drinks.
- Taking Vitamin B6 and Unisom (after consulting with your doctor).
7. What Foods Should I Eat During Pregnancy?
A balanced diet during pregnancy helps ensure your baby gets the nutrients they need. Some of the best foods to include are:
- Fruits and vegetables: Rich in vitamins, minerals, and fiber.
- Whole grains: Brown rice, oatmeal, and whole wheat bread provide energy and fiber.
- Lean proteins: Chicken, turkey, eggs, beans, lentils, and tofu support growth.
- Dairy products: Yogurt, milk, and cheese provide calcium and protein.
- Healthy fats: Avocados, nuts, seeds, and olive oil support brain development.
- Iron-rich foods: Spinach, lean meats, and fortified cereals help prevent anemia.
8. What Foods Should I Avoid?
Certain foods can pose a risk to your baby’s health and should be avoided:
- Raw or undercooked meat, eggs, and seafood (risk of bacteria and parasites like salmonella and listeria).
- Deli meats and unpasteurized dairy (can contain listeria, which can cause miscarriage).
- High-mercury fish (shark, swordfish, king mackerel, tilefish).
- Too much caffeine (limit to 200 mg/day, about one 12 oz cup of coffee).
- Alcohol (no amount is considered safe during pregnancy).
9. What Prenatal Tests Will I Need, and When?
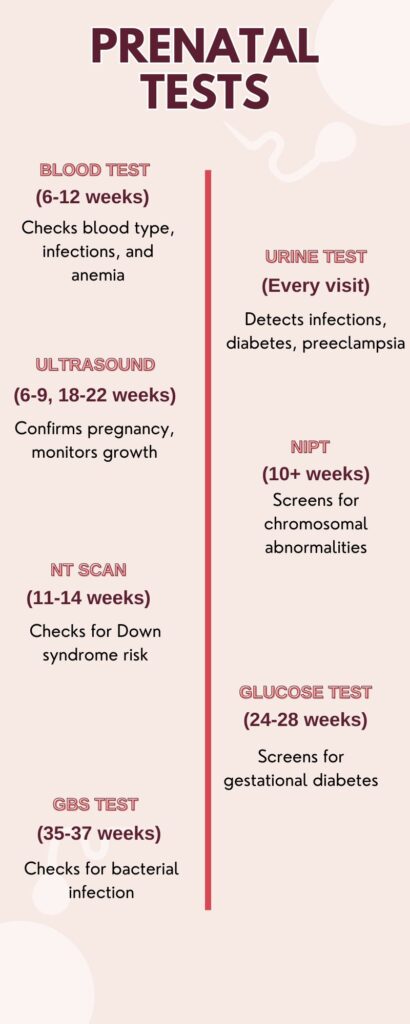
Another one of the most crucial pregnancy related frequently asked questions is about the prenatal tests. Prenatal tests help monitor your health and your baby’s development. Common tests during the first trimester include:
- Blood tests: These check for blood type, Rh factor, anemia, immunity to infections (such as rubella), and any existing conditions like diabetes or thyroid disorders.
- Urine tests: These screen for infections, protein levels, and signs of gestational diabetes.
- Ultrasound: A dating ultrasound is often done around 8-12 weeks to confirm pregnancy, check the baby’s heartbeat, and determine an estimated due date.
- Genetic screening tests (optional): These include Non-Invasive Prenatal Testing (NIPT) and First Trimester Screening to check for chromosomal abnormalities like Down syndrome.
- Pap smear and STD screening: If you haven’t had a recent Pap smear, your doctor may perform one to check for cervical health and screen for sexually transmitted infections (STIs).
10. How Much Water Should I Be Drinking Daily?
Pregnant women should aim to drink 8-12 cups (64-96 oz) of water daily. Staying hydrated helps with digestion, circulation, and amniotic fluid levels.
11. Can I Exercise During Pregnancy?
Yes! Exercise is beneficial for pregnancy, as it helps with circulation, reduces stress, and prepares your body for labor. Safe activities include:
- Walking
- Swimming
- Prenatal yoga
- Light strength training
Avoid high-impact sports, heavy lifting, or activities with a high risk of falling. Always listen to your body and modify workouts as needed.
11. Is it Okay to Travel?
Yes, most women can travel safely during the first trimester. However, if you have complications like a history of miscarriage or a high-risk pregnancy, check with your doctor first.
If flying, stay hydrated, move around every few hours, and wear a seatbelt under your belly.
12. What are Normal Pregnancy Symptoms, and When Should I be Concerned?
Normal symptoms:
- Fatigue
- Nausea/morning sickness
- Breast tenderness
- Light cramping
- Mood swings
Call your doctor if you experience:
- Heavy bleeding
- Severe pain
- High fever (over 100.4°F)
- Persistent vomiting (unable to keep fluids down)
13. What About Experiencing Spotting or Bleeding During Pregnancy?
Light spotting can be normal in early pregnancy and is often caused by implantation bleeding, hormonal changes, or cervical irritation after intercourse. However, heavy bleeding, severe pain, or clotting could indicate a more serious issue, such as a miscarriage or ectopic pregnancy. If you experience any bleeding, it’s always best to consult your doctor to rule out any complications.
14. What Genetic Tests Should I Consider Based on My Family History?
Depending on your background, you may consider:
- Carrier screening: Check if you’re a carrier for genetic disorders like cystic fibrosis, sickle cell anemia, or Tay-Sachs.
- NIPT (Non-Invasive Prenatal Testing): Screens for Down syndrome and other chromosomal conditions.
If certain conditions run in your family, your doctor may recommend additional tests.
Pregnancy Questions You Must Ask During the Second Trimester
The second trimester is often called the “honeymoon phase” of pregnancy. Morning sickness tends to fade, energy levels return, and baby movements become more noticeable. As your belly grows, so do new concerns about weight gain, prenatal screenings, and potential complications. This trimester is also the ideal time to plan ahead—whether for labor, baby essentials, or birthing preferences. Use this section to get clarity on what to expect, things to do, and how to stay healthy.
15. How Much Weight Gain is Considered Healthy During Pregnancy?
Your weight gain during pregnancy depends on your pre-pregnancy BMI (Body Mass Index). Here’s a general guideline from the American College of Obstetricians and Gynecologists (ACOG):
| Pre-Pregnancy BMI | Recommended Total Weight Gain | Weight Gain Per Week in 2nd Trimester |
| Underweight (BMI < 18.5) | 28-40 lbs (12.5-18 kg) | 1-1.3 lbs (0.45-0.59 kg) |
| Normal weight (BMI 18.5-24.9) | 25-35 lbs (11.5-16 kg) | 0.8-1 lb (0.36-0.45 kg) |
| Overweight (BMI 25-29.9) | 15-25 lbs (7-11.5 kg) | 0.5-0.7 lbs (0.23-0.32 kg) |
| Obese (BMI ≥ 30) | 11-20 lbs (5-9 kg) | 0.4-0.6 lbs (0.18-0.27 kg) |
(Source: ACOG Guidelines)
Too little weight gain can increase the risk of preterm birth and low birth weight, while excessive weight gain can lead to complications like gestational diabetes and high blood pressure.
16. How Much Weight Should I Gain?
Your exact weight gain goal depends on your body type, lifestyle, and whether you’re carrying a single baby or multiples. While the table above provides general guidelines, your doctor will help you set a target based on your personal health profile.
One thing to keep in mind is that weight gain isn’t just about fat. The extra weight comes from:
- Baby’s weight (usually 6-9 pounds at birth)
- Placenta and amniotic fluid (around 4-6 pounds)
- Increased blood volume (4 pounds)
- Breast tissue growth (2-3 pounds)
- Extra fat storage for breastfeeding and energy
As long as you’re eating a balanced diet and staying active, your weight gain will likely stay within a healthy range.
17. How to Manage Weight Gain During Pregnancy?
It’s common to worry about weight gain, but managing it doesn’t mean dieting—it means making smart food choices and staying active.
- Eat Nutrient-Rich Foods – Focus on protein, fiber, and healthy fats. Whole grains, lean meats, nuts, dairy, and fresh vegetables should be your go-to.
- Control Portion Sizes – You don’t need to eat for two! In the second trimester, your body only needs about 340 extra calories per day, which is roughly equivalent to a bowl of yogurt with granola or a peanut butter sandwich.
- Stay Active – Light exercise like walking, swimming, and prenatal yoga can help manage weight gain and improve mood.
- Hydration Is Key – Drinking at least 8-10 glasses of water a day helps prevent bloating and overeating.
18. Which Prenatal Screenings Do I Need?
The second trimester is an important time for medical screenings. These tests help monitor the baby’s growth and check for potential complications.
- The Quad Screen (15-20 weeks) – This blood test measures four substances in your blood to assess the risk of chromosomal conditions like Down syndrome and neural tube defects.
- The Anatomy Scan (18-22 weeks) – This detailed ultrasound checks your baby’s development, measuring their organs, bones, and limbs. It also determines if there are any visible abnormalities.
- Glucose Tolerance Test (24-28 weeks) – This test checks for gestational diabetes, a temporary form of diabetes that can develop during pregnancy. If diagnosed early, it can be managed with diet and lifestyle changes.
- Amniocentesis (15-20 weeks, if necessary) – A more detailed genetic test that involves drawing amniotic fluid from your uterus to test for chromosomal disorders.
Your doctor will guide you on whether you need additional tests based on your health history.
19. What Complications Can Arise This Trimester?
Another one of the most crucial pregnancy related frequently asked questions is about the complications. Although the second trimester is generally smoother than the first, certain complications can still arise, including:
- Gestational Diabetes – Affects 2-10% of pregnancies in the U.S. and can lead to a larger baby, difficult delivery, and future diabetes risk. It’s usually managed with diet.
- Preeclampsia – A dangerous condition characterized by high blood pressure, swelling, and protein in the urine. It requires immediate medical attention.
- Preterm Labor – Contractions before 37 weeks can result in premature birth. Watch for persistent cramping, lower back pain, or a sensation of pelvic pressure.
- Placenta Previa – When the placenta covers the cervix, making vaginal delivery unsafe. It often requires a C-section.
Regular prenatal check-ups help in detecting and managing these risks early.
20. Can I Continue to Work Throughout My Pregnancy?
For most women, yes! If you have a normal, healthy pregnancy and work in a safe environment, you can continue working. However, if your job involves standing for long hours, heavy lifting, or exposure to chemicals, you might need adjustments.
Tips for working while pregnant:
- Take frequent breaks – Stretch every hour if you sit for long periods.
- Stay hydrated – Keep a water bottle nearby.
- Use good posture – If sitting at a desk, use a chair with lumbar support.
- Manage stress – Take deep breaths and don’t hesitate to ask for help when needed.
If you experience excessive fatigue, dizziness, or contractions, consult your doctor about adjusting your work schedule.
21. How Can I Manage Stress During Pregnancy?
Pregnancy is an emotional rollercoaster. While some stress is normal, chronic stress can impact both you and your baby.
- Here are effective ways to stay relaxed:
Meditation & Deep Breathing – Even 10 minutes a day can lower stress.
Prenatal Yoga or Walks in Nature – Exercise releases endorphins that boost mood.
Talk About Your Feelings – Whether it’s with your partner, a friend, or a therapist, talking helps.
Get Enough Sleep – Aim for 7-9 hours of quality sleep per night.
Studies show that high stress levels during pregnancy are linked to preterm birth and low birth weight (Source).
22. Should I Be Taking Any Additional Supplements Like Iron?
Yes, additional supplements—especially iron—become crucial during the second trimester. Your body needs more iron at this stage because your blood volume is increasing to support your growing baby. Iron is essential for making hemoglobin, the protein in red blood cells that carries oxygen to your baby.
23. How Much Iron Do I Need?
The recommended daily intake of iron during pregnancy is 27 mg per day, which is almost double the amount needed for non-pregnant women.
Why Is Iron Important?
- Prevents iron-deficiency anemia, which can cause fatigue, weakness, and dizziness.
- Supports the baby’s brain development.
- Reduces the risk of preterm birth and low birth weight.
Best Sources of Iron:
- Iron-rich foods: Lean meats, poultry, fish, spinach, lentils, and fortified cereals.
- Iron supplements: If diet alone isn’t enough, your doctor may recommend an iron supplement.
💡 Pro Tip: Take iron with Vitamin C (such as orange juice) to enhance absorption. Avoid taking it with calcium-rich foods, as calcium can block iron absorption.
(Source: American Pregnancy Association)
24. What Symptoms Should I Expect?
The second trimester is often called the “honeymoon phase” of pregnancy because many early symptoms, like nausea and extreme fatigue, start to fade. However, new symptoms may appear as your body adjusts to your growing baby.
Common Symptoms in the Second Trimester:
- Baby Movements (Quickening): You may start feeling tiny kicks and flutters between 18-22 weeks.
- Increased Appetite: Your baby is growing fast, and your body needs more fuel.
- Heartburn & Indigestion: Your digestive system slows down, and your growing uterus pushes against your stomach.
- Back Pain & Round Ligament Pain: As your belly expands, your lower back and sides may ache.
- Leg Cramps & Swelling: Your body retains more fluids, leading to mild swelling in your feet and ankles.
- Dizziness or Lightheadedness: Caused by changes in blood pressure.
Most of these symptoms are normal, but if anything feels extreme, talk to your doctor.
25. When Should I Contact the Doctor?
It’s always better to be cautious when it comes to pregnancy. While most symptoms are normal, there are warning signs that require immediate medical attention.
Call your doctor immediately if you experience:
- Severe abdominal pain or cramping
- Heavy vaginal bleeding or clotting
- Sudden swelling in hands, face, or feet (sign of preeclampsia)
- Blurred vision, persistent headaches, or dizziness
- Severe back pain or painful contractions before 37 weeks
- Decreased fetal movement after 22 weeks
- High fever (over 101°F or 38.3°C)
If something doesn’t feel right, trust your instincts and call your doctor. It’s always better to be safe.
26. What Type of Exercise Is Safe for Me to Do?
Staying active during pregnancy can help with weight management, reduce stress, and prepare your body for labor. However, not all exercises are safe.
Safe Exercises for Pregnancy:
- Walking – Low-impact and easy on the joints.
- Prenatal Yoga – Improves flexibility, reduces stress, and relieves back pain.
- Swimming – Supports your weight, easing pressure on joints and back.
- Low-Impact Strength Training – Using light weights can help maintain muscle strength.
- Stationary Cycling – Safer than regular cycling because there’s no risk of falling.
Exercises to Avoid:
- High-impact sports (basketball, soccer, skiing, etc.)
- Contact sports (boxing, kickboxing, etc.)
- Heavy weightlifting that strains the abdomen
- Hot yoga or excessive stretching (risk of overheating and overstretching due to relaxin hormone)
Listen to your body. If you feel dizzy, short of breath, or experience pain, stop exercising and rest.
27. Is It Safe to Travel While Pregnant?
Yes, the second trimester (weeks 14-28) is considered the safest time to travel. Morning sickness has usually subsided, and you’re not yet in the uncomfortable third trimester.
Safe Travel Tips:
- Air Travel: Most airlines allow pregnant women to fly up to 36 weeks, but some require a doctor’s note after 28 weeks.
- Car Travel: Stop every 1-2 hours to stretch and walk around to prevent blood clots.
- International Travel: Avoid areas with Zika virus and make sure there’s quality medical care available at your destination.
- Wear compression socks on long flights to improve circulation and reduce swelling.
28. Do I Need Any Vaccinations?
During pregnancy, certain vaccines are crucial to protect both the mother and the baby from preventable diseases. Vaccination helps strengthen immunity, reduces the risk of complications, and provides essential protection to newborns in their first months of life. Below is a table outlining the most important vaccines recommended during pregnancy, along with their safety and general adult guidelines. Here are some crucial vaccines recommended during pregnancy:
| Vaccine | Vaccine Type | Pregnancy Recommendation | General Adult Recommendation |
| Influenza | Inactivated viral | 1 dose anytime during flu season | 1 dose annually |
| Tetanus Diphtheria Pertussis (Tdap/Td) | Inactivated toxoids & subunit | 1 dose after 20 weeks, preferably ~28 weeks | 1 lifetime Tdap, then Td every 10 years |
| Measles Mumps Rubella (MMR) | Live-attenuated viral | Contraindicated; 1 dose postpartum if non-immune | 1-2 lifetime doses; additional 1 dose >55 if at risk |
| Varicella | Live-attenuated viral | Contraindicated; 1 dose postpartum if non-immune | 2 lifetime doses |
29. Given My Family History, Are There Any Genetic Tests I Should Consider?
If your family has a history of genetic conditions, your doctor may recommend carrier screening for genetic testing. These tests can help determine if your baby is at risk for inherited conditions.
Common Genetic Tests:
- Carrier Screening: Tests if you or your partner carry genes for conditions like cystic fibrosis, sickle cell anemia, or Tay-Sachs disease.
- Amniocentesis (15-20 weeks): Checks for chromosomal abnormalities like Down syndrome.
- Chorionic Villus Sampling (CVS) (10-13 weeks): Another test for genetic disorders but performed earlier than amniocentesis.
Genetic counseling can help you decide if these tests are right for you.
30. What Are the Potential Risks Associated With My Family Medical History?
Your family’s medical history plays a crucial role in pregnancy care. Certain hereditary conditions could increase your risk for complications, including:
- Gestational Diabetes: If diabetes runs in your family, you may have a higher chance of developing gestational diabetes.
- Preeclampsia: A family history of high blood pressure or preeclampsia raises your risk.
- Blood Clotting Disorders (Thrombophilia): Increases the risk of deep vein thrombosis (DVT) during pregnancy.
- Genetic Conditions: Conditions like cystic fibrosis, sickle cell disease, or muscular dystrophy can be passed down to your baby.
Discussing your family history with your doctor early on helps them take the necessary precautions.
Third Trimester (Weeks 28-40)
As you enter the final stretch of pregnancy, your focus shifts toward labor, delivery, and newborn care. The third trimester brings its own set of challenges, from increased discomfort to monitoring signs of labor. Understanding birthing options, recognizing warning signs, and preparing for postpartum recovery are all essential. In this section, we answer key questions to help you feel confident, explore what things you should do, and prepare for the big day.
31. What Should I Expect During Labor?
Labor is the process your body goes through to deliver your baby. It happens in three stages:
Early and Active Labor
- Contractions begin and become more regular. They start as mild cramps and progress to stronger, longer contractions.
- Your cervix (the opening of the uterus) will thin out (efface) and open (dilate) to 10 cm.
- Early labor can last for hours or even days, while active labor (when contractions are intense and close together) lasts several hours.
Delivery of the Baby
- Once the cervix is fully dilated, you will begin pushing.
- This stage can last anywhere from a few minutes to a few hours.
- The baby’s head will emerge first (crowning), followed by the rest of the body.
Delivery of the Placenta
- After the baby is born, mild contractions will continue to help deliver the placenta.
- This usually happens within 30 minutes after birth.
Each labor experience is different, so talk to your healthcare provider about what to expect based on your health and pregnancy.
32. What Are the Signs of Preterm Labor?
Preterm labor happens before 37 weeks and can lead to premature birth, which may require extra medical care for your baby.
Signs to Watch For:
- Regular contractions that don’t stop (every 10 minutes or less).
- Lower back pain that doesn’t go away with rest.
- Cramps or pelvic pressure, similar to menstrual cramps.
- Vaginal discharge changes, including watery, mucus-like, or bloody fluid.
- Leaking fluid, which may indicate that your water has broken early.
What to Do If You Have These Signs?
Call your doctor or go to the hospital immediately. Early medical intervention may help delay labor and protect your baby’s health.
33. What Are My Birthing Options, Including Pain Management Choices?
You have several options for where and how you give birth. Understanding your choices can help you feel more confident and prepared.
Birthing Locations:
- Hospital Birth – The most common option, providing access to medical care, pain relief, and emergency interventions if needed.
- Birth Center – A home-like setting focused on natural childbirth, typically managed by midwives.
- Home Birth – Giving birth at home with a midwife or healthcare provider. This is usually recommended for low-risk pregnancies.
Pain Management Options:
- Natural Pain Relief:
- Breathing techniques (Lamaze, hypnobirthing)
- Warm baths or showers
- Movement and different labor positions
- Massage and counter-pressure
- Medical Pain Relief:
- Epidural: A common pain relief method that numbs the lower body while keeping you awake.
- Spinal Block: Similar to an epidural but used for planned C-sections.
- IV Medications: Help relieve pain but may cause drowsiness.
- Nitrous Oxide (Laughing Gas): A mild pain relief option available in some hospitals.
Talk to your doctor about what’s best for you, keeping in mind your pain tolerance and birth preferences.
34. Should I Create a Birth Plan?
A birth plan is a written document outlining your preferences for labor and delivery. While things may not always go exactly as planned, having one can help guide your medical team and ensure your wishes are considered.
What to Include in Your Birth Plan:
- Pain management preferences (epidural, natural methods, or a combination).
- Labor positions you’d like to try (walking, squatting, birthing ball).
- Who will be present (partner, family, doula, or just medical staff).
- Immediate newborn care (skin-to-skin contact, delayed cord clamping, breastfeeding).
A flexible mindset is key, as birth can be unpredictable.
35. What Are the Risks and Benefits of a Vaginal Birth vs. a C-Section?
Both delivery methods have advantages and risks. But no doubt, normal delivery is the best way to give birth. Your doctor will help determine what’s safest for you and your baby.
Vaginal Birth:
✅ Benefits:
- Faster recovery time (usually within a few weeks).
- Lower risk of complications in future pregnancies.
- Immediate skin-to-skin contact and early breastfeeding initiation.
⚠️ Risks:
- Possibility of tearing or needing an episiotomy (a small surgical cut).
- Longer labor, especially for first-time moms.
- Risk of emergency C-section if complications arise.
C-Section (Cesarean Delivery):
✅ Benefits:
- Can be planned for medical reasons (e.g., breech baby, placenta previa).
- Less risk of birth trauma (such as head or shoulder injuries for the baby).
⚠️ Risks:
- Longer recovery (about 6-8 weeks).
- Increased risk of infection and complications in future pregnancies.
- Higher likelihood of breathing issues for the baby.
Discuss your options with your doctor, especially if you have a high-risk pregnancy.
36. What is Painless Delivery?
Painless delivery refers to childbirth with epidural anesthesia, which numbs pain while allowing the mother to stay awake and participate in labor. The epidural is administered in the lower back and takes 10-15 minutes to work, offering significant pain relief.
Benefits:
- Less labor pain and stress
- More energy for pushing
- Controlled, relaxed birth experience
Possible Side Effects:
- Temporary leg numbness
- Mild drop in blood pressure
- Back soreness
It’s a safe option for many mothers, but consult your doctor to see if it’s right for you!
37. How Can I Prepare for Breastfeeding?
Well, there are several myths related to breastfeeding. However, it is a natural process, but it can take time to learn. Here’s how to get ready:
- Take a breastfeeding class to learn about latching, positioning, and common challenges.
- Invest in breastfeeding essentials like a nursing pillow, breast pump, and nipple cream.
- Talk to a lactation consultant before birth to address any concerns.
- Know your baby’s feeding cues (rooting, sucking on hands, fussiness).
What Should I Know About Breastfeeding?
- Colostrum (first milk) is packed with nutrients and antibodies. It’s often yellowish and thick.
- Milk production increases after a few days when your mature milk comes in.
- Newborns need to nurse frequently (8-12 times per day).
- A good latch is crucial to avoid nipple pain and ensure proper feeding.
- Hydration and a balanced diet help maintain a healthy milk supply.
If you encounter difficulties, lactation consultants can provide guidance and support.
38. What Complications Can Arise This Trimester?
Some potential third-trimester complications include:
- Preeclampsia: High blood pressure, swelling, and protein in the urine—can be life-threatening if untreated.
- Gestational Diabetes: Can lead to a larger baby and delivery complications.
- Placenta Previa: When the placenta covers the cervix, often requiring a C-section.
- Preterm Labor: Delivering before 37 weeks can pose risks to the baby.
Regular prenatal checkups can help catch these issues early.
39. Is It Okay to Travel During the Third Trimester?
Flying:
- Most airlines allow travel until 36 weeks but may require a doctor’s note.
- Drink plenty of water and move frequently to prevent blood clots.
- Have your medical records handy in case of emergencies.
Long Car Rides:
- Take breaks every 1-2 hours to stretch and walk.
- Wear a seatbelt below your belly for safety.
General Guidelines:
- Avoid destinations with poor medical facilities or high altitudes.
- Stay close to a hospital in case labor starts early.
If you have complications, your doctor may advise against travel.
Final Thoughts
Pregnancy is a life-changing journey filled with excitement, joy, and, sometimes, a bit of uncertainty. While this list of pregnancy related frequently asked questions covers essential aspects of each trimester, every pregnancy is unique. Your experience may differ from someone else’s, and that’s completely normal.
The most important thing is to stay informed, listen to your body, and maintain open communication with your doctor. Whether it’s understanding prenatal care, managing symptoms, or preparing for labor and delivery, asking the right questions ensures a healthy pregnancy and a smooth transition into motherhood.
Remember, you don’t have to go through this journey alone—your healthcare provider, partner, family, and support network are there to guide you every step of the way. Embrace this special time, trust the process, and enjoy the beautiful experience of bringing new life into the world!




